Blood clots save lives….until they don’t. The same process that stops a paper-cut from bleeding can, in the wrong place, block blood flow to the brain, heart, or lungs. That’s where anticoagulants, commonly known as blood thinners, come in. These powerful medications keep your blood flowing smoothly and are lifesavers for people with conditions like deep vein thrombosis (DVT), pulmonary embolism (PE), and atrial fibrillation (AF).
But like every hero, they have their flaws. Managing anticoagulants requires precision, vigilance, and a good understanding of how they work. In this blog, let’s explore how these drugs prevent dangerous clots, how different classes function, and what challenges pharmacists and clinicians face in using them safely.
Types of Anticoagulants
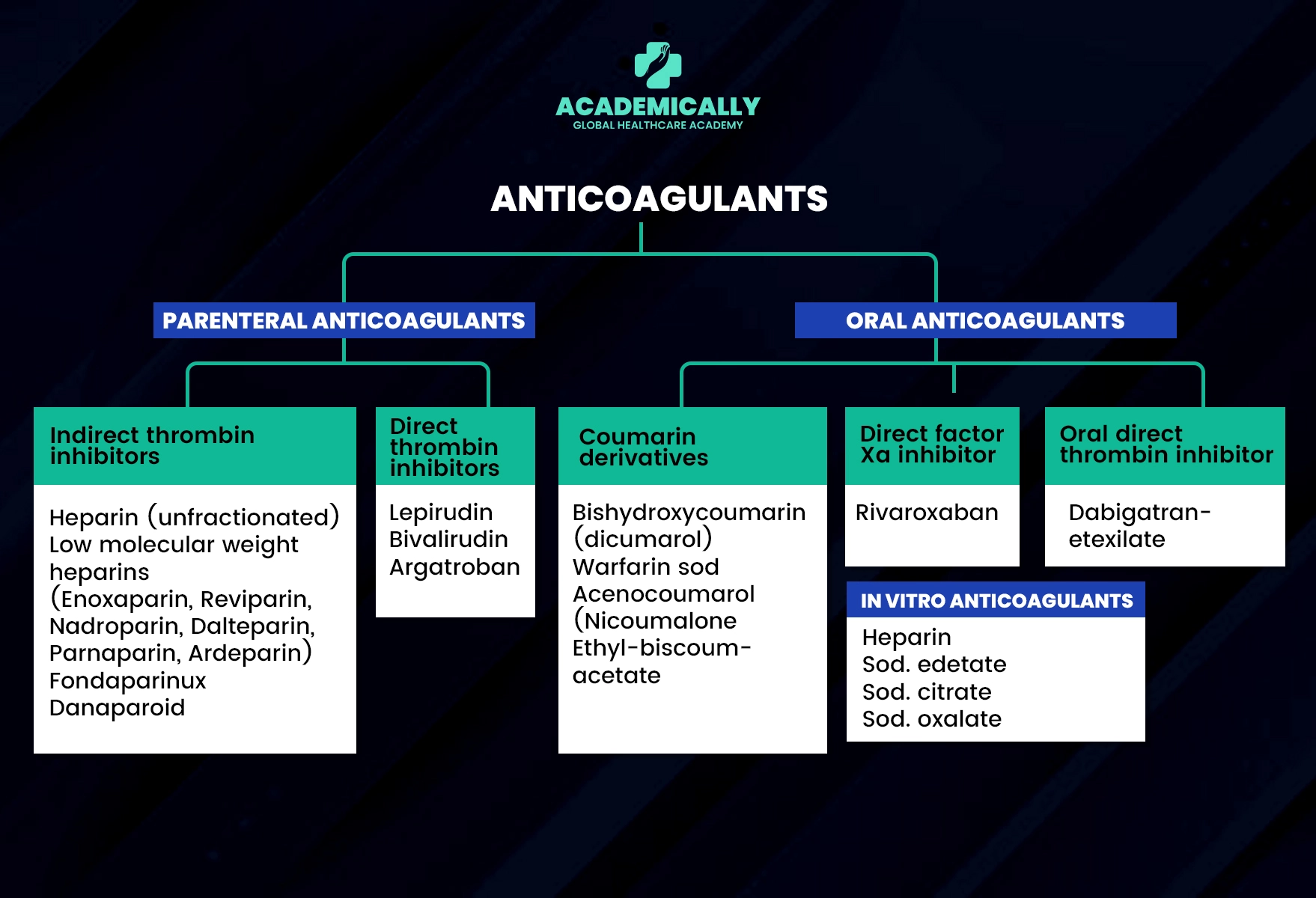
Here are some of the important classes of Anticoagulants and their mechanisms.
- Vitamin K Antagonists (VKAs)
- Example: Warfarin
- Mechanism: VKAs inhibit vitamin K epoxide reductase, an enzyme necessary for the synthesis of clotting factors II, VII, IX, and X. By reducing the levels of these factors, VKAs effectively decrease blood clotting.
- Considerations: Warfarin requires regular monitoring of the International Normalised Ratio (INR) to ensure therapeutic levels and minimise the risk of bleeding or clotting complications. Dietary interactions, especially with vitamin K-rich foods, can also affect warfarin’s efficacy.
- Direct Oral Anticoagulants (DOACs)
- Examples: Apixaban, Rivaroxaban, Dabigatran, Edoxaban
- Mechanism: DOACs target specific coagulation factors directly. For instance, apixaban and rivaroxaban inhibit Factor Xa, while dabigatran inhibits thrombin (Factor IIa). This direct action reduces clot formation without the need for routine monitoring.
- Considerations: DOACs have fewer dietary restrictions and interactions compared to VKAs, but they still require careful management, especially in patients with renal impairment. Reversal agents for DOACs are available but vary among the drugs.
- Heparins
- Examples: Unfractionated Heparin (UFH), Low Molecular Weight Heparins (LMWH) such as Enoxaparin
- Mechanism: Heparins enhance the activity of antithrombin III, which inactivates thrombin and Factor Xa, thereby preventing clot formation. UFH is typically administered intravenously, while LMWH is given subcutaneously.
- Considerations: Heparins require monitoring of activated partial thromboplastin time (aPTT) for UFH, while LMWH generally does not need routine monitoring. Bleeding risks and heparin-induced thrombocytopenia (HIT) are significant concerns.
Challenges Faced During Anticoagulant Therapy
Let's take a look at the challenges faced during therapy with these drugs.
- Risk of Bleeding: All anticoagulants carry a risk of bleeding, which can be severe or life-threatening. Managing this risk involves balancing the therapeutic benefits against the potential for adverse effects.
- Drug Interactions: Anticoagulants interact with various medications, including other anticoagulants, antiplatelets, and certain antibiotics. These interactions can either enhance the anticoagulant effect or reduce its efficacy.
- Reversal and Management of Complications: Effective management of bleeding complications or overdose involves the use of reversal agents or supportive treatments. The availability and effectiveness of these agents vary among different anticoagulants.

The Future of Anticoagulant Therapy
Anticoagulant therapy is getting better with new research focusing on safer drugs. To sum it up, these medications are key for managing blood clots. Understanding how they work and staying updated on new developments are important for providing the best patient care
Anticoagulants are one of the key topics frequently covered in the OPRA exam. Understanding their mechanisms, uses, and challenges is essential for scoring well and applying knowledge in real-world clinical settings.
At Academically, we help you master such high-yield subjects through expert-led sessions, study materials, and comprehensive guidance designed to help you excel with confidence.






