Have you ever wondered what happens to a drug when it enters our system? When you take medicine for something as simple as a headache, it goes through a lengthy process in the body before it shows its action. This process is called the ADME profile of the drug. Or, in simple words, how the body treats the drug.
The ADME profile influences not only how the drug acts in the body, but also how we prepare the formulation and the mode of administration.
In this blog, we will go through the basics of ADME.
So pick up your pen and paper, and start taking notes.
What is ADME?
ADME stands for adsorption, distribution, metabolism and excretion of the drug in the body. Absorption gets the drug into your bloodstream. Distribution carries it to where it's needed. Metabolism breaks it down, and excretion flushes it out. These are the four main points that decide if a drug:
- Works well
- Lasts long enough, or
- Causes side effects
It directly shapes its power and safety.
It is important to get ADME right early in drug development. It cuts failures in human trials by spotting issues like poor uptake or quick breakdown. Scientists use lab tests, animal models, and computer predictions to tweak drugs for better performance.
Let’s look at the steps in detail.
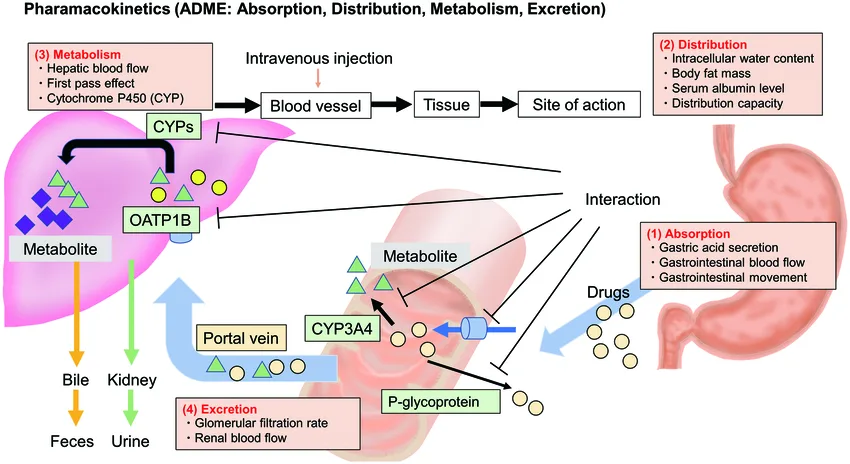
Absorption: The First Hurdle
This first step moves drugs from entry points like the gut, skin, or lungs into blood.
- Oral pills battle stomach acid and enzymes.
- Fat-soluble and smaller molecules slip through easier.
Different routes also change the absorption.
- Inhaled medications reach the lungs quickly
- Injections bypass hurdles for quick relief.
- Food, pH, or gut pumps can speed or stall absorption.
Poor uptake means low levels at work sites, making therapies useless. Nanoparticles boost this by 30% in studies via better gut crossing.
Distribution: Reaching The Target
Once in the blood, distribution spreads the drug to organs and tissues. Blood now shuttles drugs to tissues through flow, diffusion, or carriers. Protective barriers, such as the blood-brain barrier, keep most drugs out of sensitive areas unless specially designed to cross.
Key factors at play:
- Fat-loving drugs reach the brain or stores. Water-types stay in fluids.
- Proteins bind drugs like taxis. Free ones act, bound ones wait.
High spreading drugs, or those having a high Vd, are widely distributed in the body. Those with low Vd are kept bound to the blood.
Inflammation causes leaks in blood vessels. This helps in pulling extra drug to the sore spots like joints.
Metabolism: Body's Transformer
The main driver of metabolism is the liver which uses CYP450 enzymes to tweak drugs for easy exit. This makes them more water-soluble and ready for removal.
There are two main phases:
- Phase I adds groups like oxygen for change.
- Phase II tags on sugars for water-friendliness.
Your genetic makeup also affects the speed of metabolism. If you have a slow metabolism, you might get drug buildup and side effects. People with faster metabolism are able to clear the drug quickly.
Smoking or antibiotics also interact with the metabolism process. They have altering effects like caffeine buzz or statin risks.
The first-pass metabolism by the liver is the biggest factor of lowering the bioavailability of oral drugs.
Excretion: The Final Cleanup
Excretion eliminates drug remnants, primarily through the kidneys into urine or the liver into bile and stool.
Main routes:
- In the kidney, the glomeruli grab small free drugs while the tubes tweak reabsorption.
- Lungs exhale volatile drugs like anaesthetics
- Other minor paths include sweat or milk.
- The recycling loop extends the action of some drugs like contraceptives.
Kidney issues in elders prolong the stay of the drug in the body, requiring dose adjustments.
The half-life of the drug dictates dosing schedules. Ones with short half-life need frequent repeats, while long ones risk toxic buildup if overused.
Why ADME Shapes Drug Action
The ADME profile of the drug is linked to power and safety every time.
- Slow absorption delays relief.
- Wide-spread drugs target tumors but can harm the heart.
- Rapid metabolism shortens antibiotic coverage.
- Poor exit leads to piling up of drugs in patients with compromised livers..
- Predictive tools screen thousands of candidates early and save billions in development costs.
Newer biologics, like antibody drugs, alter ADME through modifications such as PEGylation. This extends the drug circulation for weekly dosing instead of daily. Diseases reshape the rules too. Inflamed tissues absorb more drugs. Immune responses, on the other hand, clear biologics faster.
Mastering ADME leads to personalized dosing, better trials, and safer therapies for everyone.
ADME Basics At A Glance
| ADME step | Main determinants | Clinical consequences |
| Absorption | Solubility Formulation pKa First-pass metabolism | Low bioavailability results in higher/alternative dosing |
| Distribution | Lipophilicity Protein binding Tissue perfusion | Alters onset/duration Affected by disease |
| Metabolism | CYPs Conjugation enzymes Genetics Drug interactions | Variable clearance Active/toxic metabolites |
| Excretion | Renal/biliary function Urine pH | Dose adjustments in kidney/liver disease |
Effective Tips for Remembering and Applying ADME
- When in doubt, check the free fraction. Only unbound drugs are active and cleared.
- Think CYPs for interactions. If a drug is a known CYP substrate, check for inhibitors and inducers.
- Use predictive tools early. In drug discovery and project work, simple in-silico predictors and ADME screens help flag problems early.
- Adjust for liver disease if metabolism is a major route. Adjust for kidney disease if renal excretion is significant.
ADME: The Science Behind Drug Behaviour
ADME is where a molecule’s chemistry meets human biology. A great drug on paper can fail in the body if it’s
- Not absorbed
- Too rapidly metabolized, or
- Accumulates to toxic levels
On the other hand, clever formulation or understanding of metabolism can turn a weak molecule into a successful medicine.
For students and practitioners, thinking in ADME terms makes pharmacology practical. It explains why dose matters, why interactions occur, and how to tailor therapy safely.
ADME is also an important part of both your pharmacy and medical curriculum. For exams like OPRA, AMC, or even FMGE, this is one topic you should not miss.






