Dentinogenesis imperfecta
Dentinogenesis imperfecta is an autosomal dominant condition affecting both deciduous and permanent teeth. Affected teeth are grey to yellowish brown and have broad crowns with constriction of the cervical area, resulting in a tulip shape.
Cause
Classification
- Dentinogenesis imperfecta I: Dentinogenesis imperfecta without osteogenesis imperfecta (opalescent dentin) corresponds to dentinogenesis imperfecta type II of Shields classification.
- Dentinogenesis imperfecta II: brandywine type, dentinogenesis imperfecta: this correspondence to dentinogenesis imperfecta type III of Sheilds classification.
Clinical features
Here are the clinical features of dentinogenesis imperfecta I and dentinogenesis imperfecta II.
Dentinogenesis imperfecta I
(Opalescent dentin, dentinogenesis imperfecta without osteogenesis imperfecta, opalescent teeth without osteogenesis imperfecta, dentinogenesis imperfecta, Shields type III, Capadepont teeth)
- The teeth are blue-grey or amber-brown and opalescent.
- The usual scalloping of the dentin enamel junction is absent.
- The teeth are shorter than normal, often markedly in respect to the roots and crowns. In some cases, a total crown is lost.
Dentinogenesis imperfecta II
(Shields type III, Brandywine type dentinogenesis imperfecta)
- The crowns of the deciduous and permanent teeth wear rapidly after the eruption, and multiple pulp exposures may occur.
- The dentin is amber and smooth.

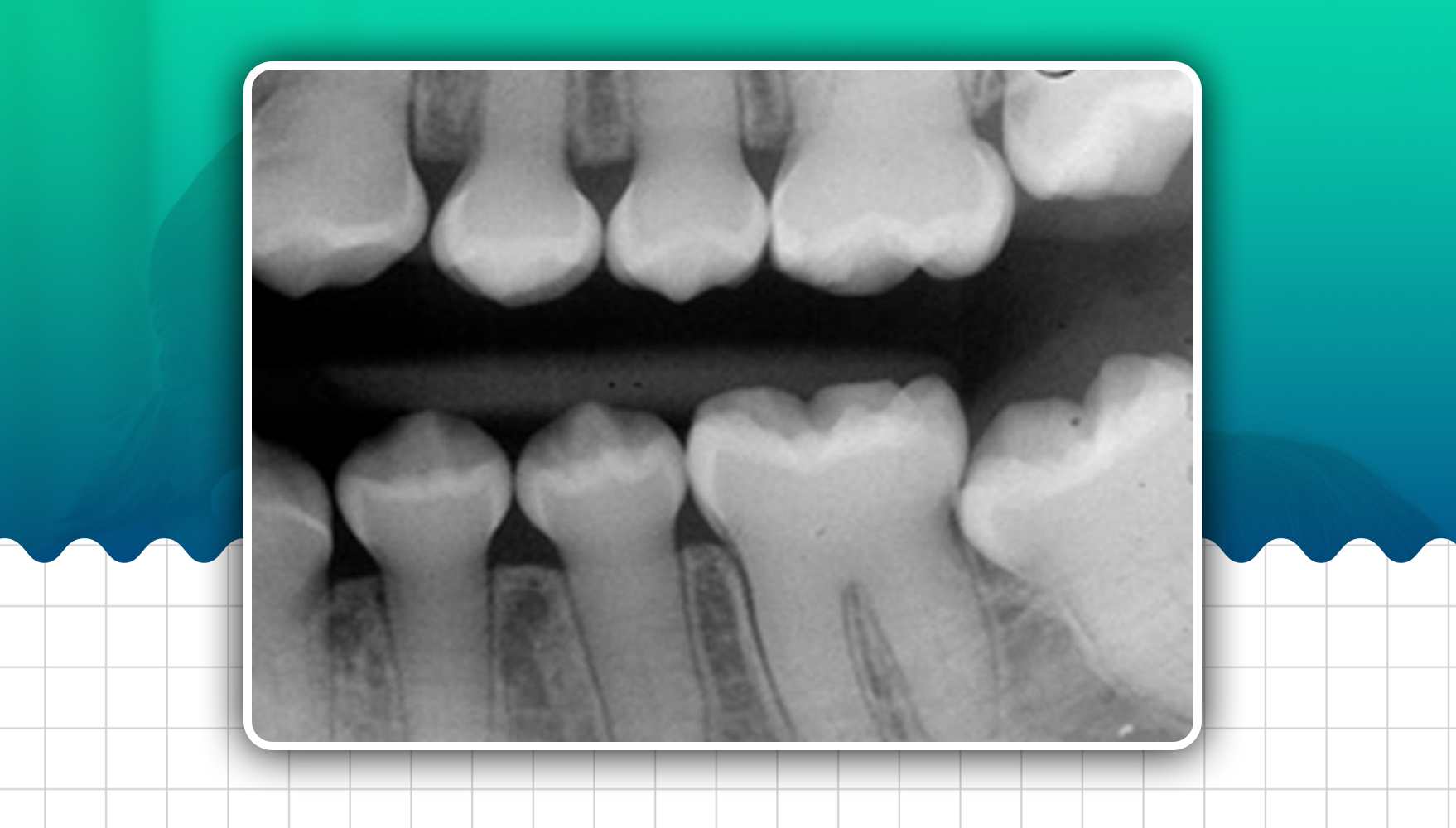
Radiographic features
- Constriction of the cervical portion of the tooth that imparts a bullous appearance
- There may be slight to marked attrition of teeth, pulp, root and root canal: Partial or complete obliteration of pulp chamber. Pulp obliteration may take place before or after the eruption of teeth. Root canals may be absent or thread-like or may be blunted.
- Periapical radiolucency without pulpal involvement and periodontal ligament space widening
- Flame-shaped pulp canal: In some cases, the radicular portion of pulp cavities is very narrow, while the pulp chambers have a bulbous expansion terminating in a point deep to the occlusal aspect, which resembles 'flame.'
- Shell teeth: In Brandywine type, the tooth's enamel appears normal, while the dentin is extremely thin, and the pulp chambers are enormous. Teeth appear as 'shell teeth'. In addition, the tooth's roots are extremely short, so it seems as if enamel and dentin are surrounded by extremely large pulp chambers and root canals.
Histological Features
The histological appearance of teeth in dentinogenesis imperfecta I emphasises that this is purely a mesodermal disturbance.
- The appearance of enamel is normal except for its peculiar shade, which is a manifestation of the dentinal disturbance.
- The dentin is composed of irregular tubules, often with large areas of uncalcified matrix.
- The tubules tend to be larger in diameter and thus more numerous than normal in a given volume of dentin.
- In some areas, there may be a complete absence of tubules.
- The continued deposition of dentin obliterates the pulp chamber.
- The odontoblasts cannot form a well-organised dentinal matrix and appear to degenerate readily, becoming entrapped in the matrix.
Chemical and physical features
- The water content is significantly increased, as much as 60% above normal, while the dentin's inorganic content is less than normal.
- Dentin density, X-ray absorption, and hardness are also low.
Diagnosis
- Clinical diagnosis: Rapid loss of enamel with attrition of tooth. Clinically, multiple pulp exposure can be seen.
- Radiological diagnosis: Obliteration of pulp chamber. Presence of periapical radiolucency without pulpal involvement.
Treatment
The treatment of patients with dentinogenesis imperfecta is directed primarily towards preventing the loss of enamel and subsequent loss of dentin through attrition.
- Overdenture: Overdenture should be given, and teeth should be covered with fluoride-releasing glass ionomer cement.
- Crown: Cast metal crown in posterior and jacket crown in anterior can be given. Caution must be exercised when using partial appliances that exert stress on the teeth.
Final Words
To learn more about this topic and prepare for the ADC exam, consider enrolling into the ADC Exam Preparation Course.
Please complete this form to get one-on-one counselling with one of our experts about the ADC exam and course.