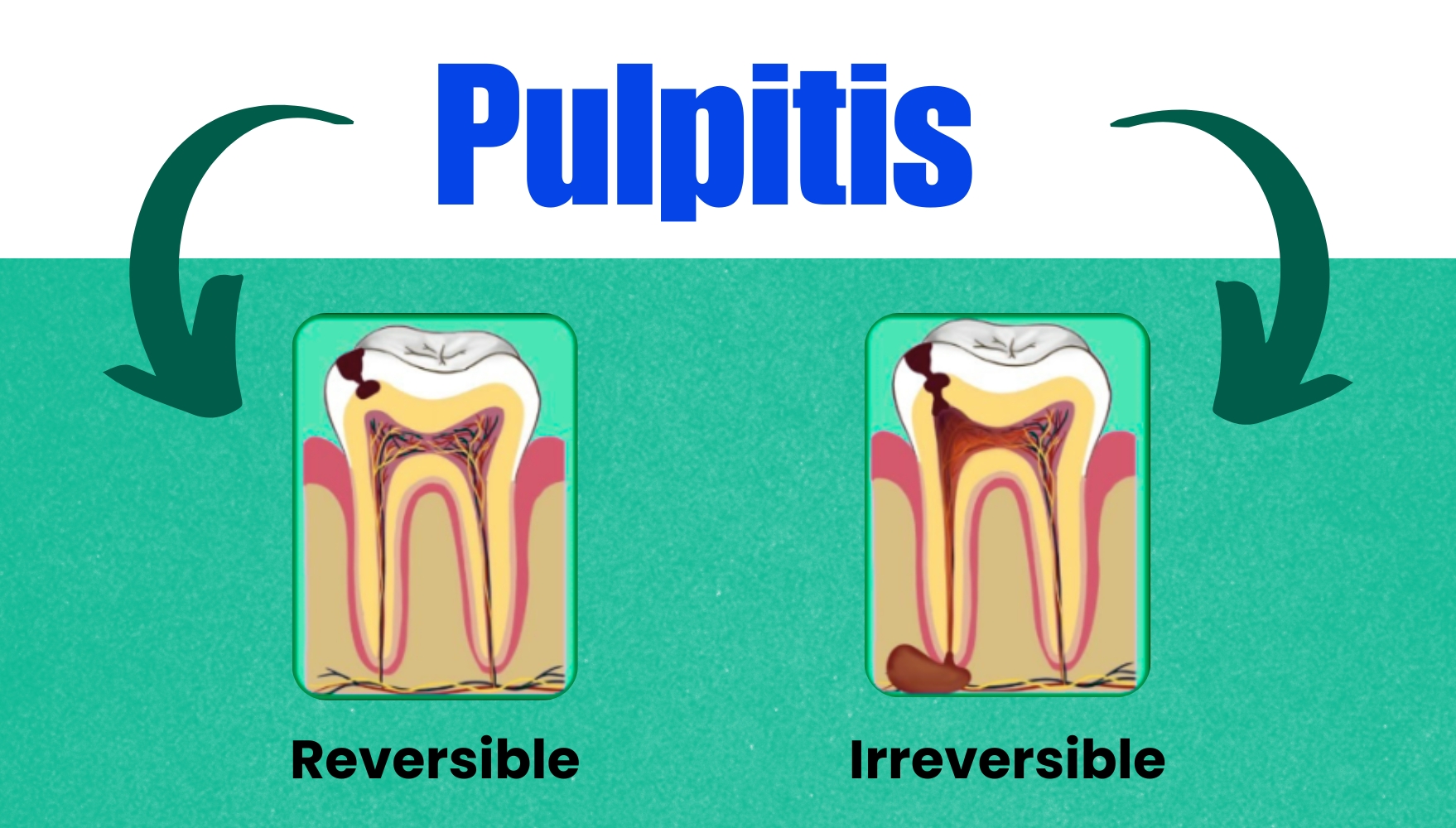
Reversible Pulpitis
This is the first stage in which the pulp is symptomatic. There is a sharp, hypersensitive response to cold, but the pain subsides when the stimulus is removed. The patient may describe symptoms of momentary pain and cannot locate the source of pain. This stage can last for months or years.
Definition
Reversible pulpitis is a mild-to-moderate inflammatory condition of the pulp caused by noxious stimuli in which the pulp can return to its normal state following the removal of stimuli.
It is an indication of peripheral A-delta fibre stimulation. Determination of reversibility is the clinical judgment that is influenced by the history of the patient and clinical evaluation.
Etiology
Pulpal irritation to external stimuli is related to dentin permeability. Under normal circumstances, enamel and cementum act as an impermeable barrier to block the patency of dentinal tubules at dentinoenamel junction or dentino- cemental junction.
Dentinal tubules become permeable when caries and operative procedures interrupt this natural barrier. So, inflammation can be caused by any agent capable of injuring pulp. It can be:
- Trauma
- Accident or occlusal trauma
- Thermal injury
- While tooth preparation with dull bur without coolant.
- Overheating during polishing of a restoration.
- Keeping bur in contact with teeth too long.
- Chemical stimulus-like sweet or sour foodstuff Following insertion of a deep restoration, the patient often complains of mild sensitivity to temperature changes, especially cold. Such sensitivity may last for 2 to 3 days, a week, or longer but gradually, it subsides. This sensitivity is symptomatic of reversible pulpitis.
Symptoms
- Reversible pulpitis is characterised by sharp pain lasting for a moment, commonly caused by cold stimuli.
- Pain does not occur spontaneously and does not continue when an irritant is removed.
- It may result from incipient caries and is resolved by removing caries and properly restoring the tooth.
Histopathology
Reversible pulpitis may range from hyperemia to mild to moderate inflammatory changes limited to the area of involved dentinal tubules. It shows:
- Increased blood volume of pulp associated with increased intrapulpal pressure.
- Edema of tissue.
- White cell infiltration.
- Reparative dentin formation.
Diagnosis
Patient's symptoms and clinical tests.
- Pain: It is sharp but of brief duration, ceasing when an irritant is removed. It is usually caused by cold, sweet and sour stimuli.
- Visual examination and history: May reveal caries, traumatic occlusion and undetected fracture.
- Radiographs:
- Show normal PDL and lamina dura, in other words, normal periapical tissue.
- Depth of caries or restoration may be evident.
- Percussion test: Shows negative response, i.e. tooth is normal to percussion and palpation without any mobility.
- Vitality test: Pulp responds readily to cold stimuli. An electric pulp tester requires less current to cause pain.
Treatment
- The best treatment of reversible pulpitis is prevention.
- No endodontic treatment is needed for this condition.
- Usually, a sedative dressing is placed, followed by permanent restoration when symptoms completely subside. Periodic care to prevent caries, desensitisation of hypersensitive teeth, and use of cavity varnish or base before insertion of restoration are recommended.
- If pain persists despite proper treatment, pulpal inflammation should be considered irreversible and treated by pulp extirpation.
Features | Reversible Pulpitis | Irreversible Pulpitis |
| Pain Type | Sharp and fleeting pain usually dissipates after the stimulus is removed | Intense, continuous and prolonged pain due to pressure and secondary irritants |
| Stimulus | External stimuli, for example, heat, cold and sugar | No external stimulus Dead or injured pulp tissue acts as a secondary stimulant |
| Pain at night/postural | No | Yes |
| Pain localisation | Only with applied cold stimulus or PDL inflammation | Only with applied heat stimulus or PDL inflammation |
| Referred Pain | Usually not found | Common |
| History | History of recent dental procedure Sometimes cervical erosion/abrasion | History of: Trauma Extensive restoration |
| Percussion/occlusion | If due to occlusion, percussion is positive, otherwise normal | If inflamed, the involved PDL-percussion test is positive otherwise, normal |
Pulp Tests
|
Normal response Exagerrated response Normal-exagerrated response |
Normal to elevated response Pain relieved by cold occasionally Acute pain |
| Colour change | No | Yes |
| Radiograph | Caries, defective restoration without pulp protection | Caries, defective restorations, PDL enlargement |
| Treatment | Removal of decay, repair of defect, restoration, ZOE dressing, occlusal adjustment | Pulpectomy (single root), a pulpotomy (multple roots), occlusal adjustment |
Irreversible Pulpitis
Definition
It is a persistent inflammatory condition of the pulp, symptomatic or asymptomatic, caused by a noxious stimulus". It has both acute and chronic stages in pulp.
Etiology
- The most common cause of pulpitis is bacterial involvement of pulp through caries.
- Chemical, thermal, and mechanical injuries of pulp may induce pulp inflammation.
- Reversible pulpitis, when left untreated, deteriorates into irreversible pulpitis.
Symptoms
- A rapid onset of pain can be caused by sudden temperature changes, sweet or acidic food. Pain remains even after the removal of the stimulus.
- Pain can be spontaneous, sharp, piercing, intermittent, or continuous in nature.
- Pain is exacerbated when bending down or lying down due to changes in intrapulpal pressure.
- Presence of referred pain.
- In later stages, pain is severe, boring, and throbbing in nature, increasing with hot stimulus. It is so severe that it keeps the patient awake at night. Pain relief can be achieved simply by using cold water. The patient may report to the dental office with a jar of ice water.
Diagnosis
- Visual examination and history: Examining the involved 9 teeth may reveal previous symptoms. On inspection, one may see a deep cavity involving pulp or secondary caries under restorations.
- Radiographic findings:
- It may show the depth and extent of caries
- The periapical area shows normal appearance, but a slight widening may be evident in advanced stages of pulpitis.
- Percussion: Tooth is tender on percussion (due to increased intrapulpal pressure as a result of exudative inflammatory tissue)
- Vitality tests
- Thermal test: Hyperalgesic pulp responds more readily to cold stimulation than normal tooth pulp; pain may persist even after removal of the irritant.
- As the pulpal inflammation progresses, heat intensifies the response because it has an expansible effect on blood vessels. Cold relieves pain because of its contractile effect on vessels, reducing the intrapulpal pressure.
- Electric test: Less current is required in the initial stages. As the tissue becomes more necrotic, more current is required to generate the response.
Treatment
A pulpectomy, i.e. root canal treatment.
Final Words
A comprehensive understanding of reversible and irreversible pulpitis is vital for dental professionals, particularly those preparing for the ADC exam. This knowledge ensures accurate diagnosis and effective treatment, preventing complications and enhancing patient care.
If you want practice questions on this topic or any other important topics for ADC, join Academically’s ADC Exam Preparation Course. Apart from study materials and question banks, you will also get guidance throughout the exam preparation from ADC-qualified mentors.
For more information, fill out this form for one-on-one counselling with our expert.