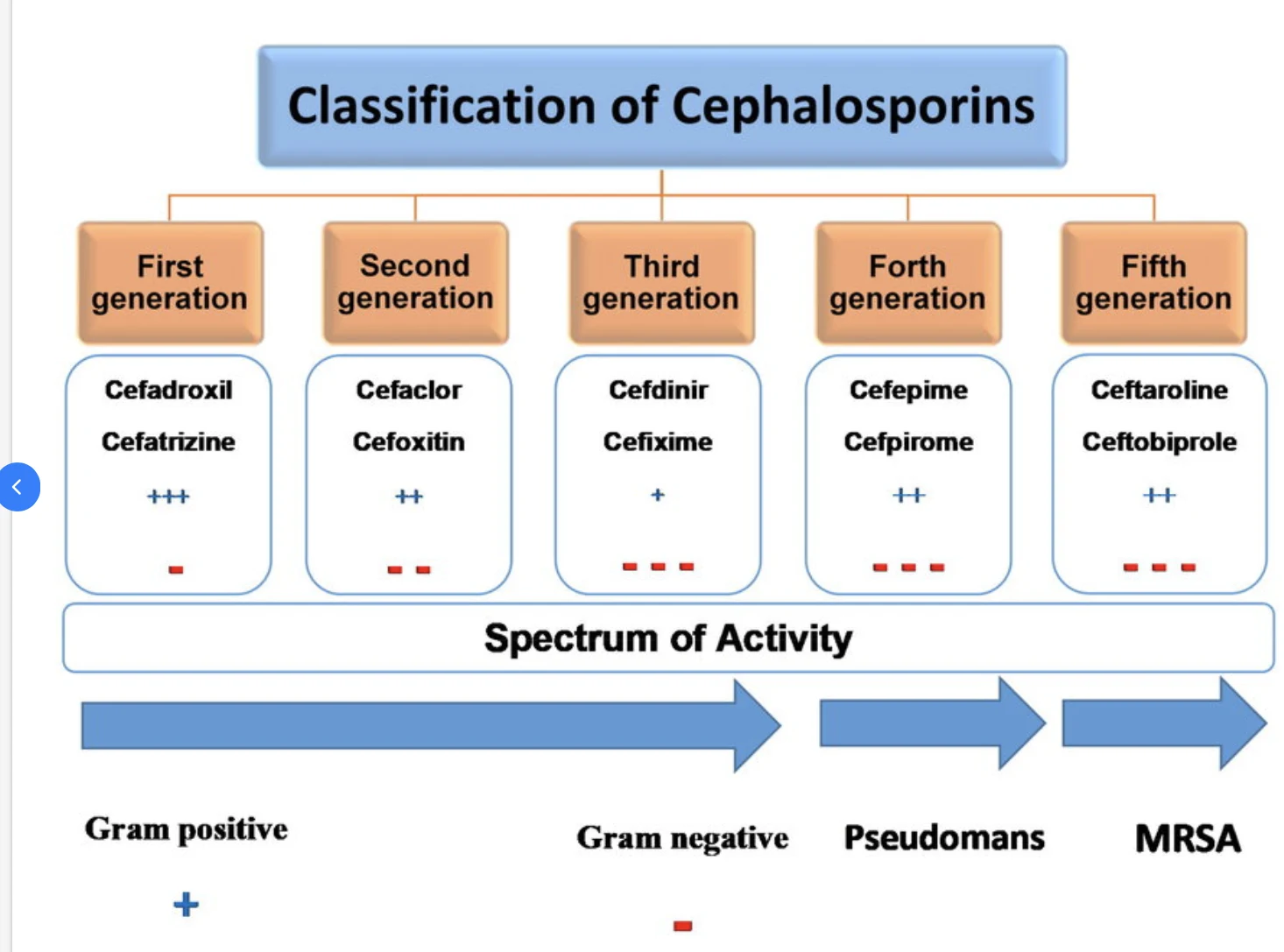
Classification of Cephalosporins
Cephalosporins are classified into five generations based on their antimicrobial spectrum and resistance to beta-lactamases, enzymes produced by bacteria that can inactivate antibiotics.
- First-Generation Cephalosporins: These include drugs like cephalexin and cefazolin. They are primarily effective against gram-positive bacteria, such as Staphylococcus and Streptococcus species. First-generation cephalosporins are commonly used for skin and soft tissue infections, as well as for surgical prophylaxis.
- Second-Generation Cephalosporins: Examples include cefuroxime and cefaclor. These have a broader spectrum of activity, covering both gram-positive and some gram-negative bacteria. They are often used to treat respiratory tract infections, including pneumonia and bronchitis, as well as urinary tract infections.
- Third-Generation Cephalosporins: Drugs like ceftriaxone and cefotaxime belong to this generation. They have an even broader spectrum of activity, including greater efficacy against gram-negative bacteria. Third-generation cephalosporins are widely used for more severe infections, such as meningitis, sepsis, and complicated urinary tract infections.
- Fourth-Generation Cephalosporins: Cefepime is a notable example of a fourth-generation cephalosporin. It has enhanced activity against both gram-positive and gram-negative bacteria, including those resistant to earlier generations. Fourth-generation cephalosporins are reserved for serious hospital-acquired infections, such as pneumonia and intra-abdominal infections.
- Fifth-Generation Cephalosporins: The newest addition to the cephalosporin family, fifth-generation drugs like ceftaroline and ceftobiprole, are effective against multidrug-resistant bacteria, including Methicillin-resistant Staphylococcus aureus (MRSA). They are primarily used for treating skin infections and community-acquired pneumonia.
Mechanism of Action
Cephalosporins act by inhibiting the synthesis of bacterial cell walls. They achieve this by binding to specific proteins known as penicillin-binding proteins (PBPs), which play a crucial role in the formation of the bacterial cell wall. By inhibiting PBPs, cephalosporins prevent the cross-linking of peptidoglycan chains, which are essential components of the bacterial cell wall. As a result, the integrity of the cell wall is compromised, leading to bacterial cell lysis and death.
Clinical Uses
Cephalosporins are used to treat a wide range of infections caused by susceptible bacteria. Their versatility and broad-spectrum activity make them a go-to choice for many clinicians. Some of the common clinical uses of cephalosporins include:
- Respiratory Tract Infections: Cephalosporins are frequently prescribed for respiratory infections such as pneumonia, bronchitis, and sinusitis. Second and third-generation cephalosporins are particularly effective against pathogens like Haemophilus influenzae and Streptococcus pneumoniae.
- Skin and Soft Tissue Infections: First-generation cephalosporins, like cephalexin, are often used to treat skin infections, including cellulitis and impetigo, caused by gram-positive bacteria.
- Urinary Tract Infections (UTIs): Second and third-generation cephalosporins are commonly used for UTIs, especially in cases where resistance to other antibiotics, such as penicillins, is a concern.
- Bone and Joint Infections: Cephalosporins are effective in treating osteomyelitis and septic arthritis, often caused by Staphylococcus aureus. Third-generation cephalosporins, like ceftriaxone, are typically used for these infections.
- Meningitis: Third-generation cephalosporins, such as ceftriaxone and cefotaxime, are the drugs of choice for bacterial meningitis due to their ability to penetrate the blood-brain barrier and effectively target the causative pathogens, including Neisseria meningitidis and Streptococcus pneumoniae.
- Surgical Prophylaxis: First-generation cephalosporins, particularly cefazolin, are widely used to prevent surgical site infections. They are administered preoperatively to reduce the risk of postoperative infections caused by skin flora.
- Hospital-Acquired Infections: Fourth-generation cephalosporins, like cefepime, are often used to treat severe hospital-acquired infections, including pneumonia, sepsis, and intra-abdominal infections. Their broad-spectrum activity makes them suitable for empiric therapy in critically ill patients.
- Multidrug-Resistant Infections: Fifth-generation cephalosporins, such as ceftaroline, are used to treat infections caused by multidrug-resistant bacteria, including MRSA. They are particularly useful in cases where other antibiotics have failed.
Potential Side Effects
Like all antibiotics, cephalosporins can cause side effects, although they are generally well-tolerated. Some of the common side effects include:
- Gastrointestinal Issues: Nausea, vomiting, diarrhoea, and abdominal pain are common gastrointestinal side effects associated with cephalosporins. These symptoms are usually mild and resolve on their own.
- Allergic Reactions: Some individuals may develop allergic reactions to cephalosporins, ranging from mild rashes to severe anaphylaxis. Patients with a known allergy to penicillins may also be at risk of cross-reactivity with cephalosporins, although this risk is relatively low.
- Clostridium difficile Infection: Cephalosporins, particularly broad-spectrum agents, can disrupt the normal gut flora, leading to an overgrowth of Clostridium difficile, a bacterium that causes severe diarrhoea and colitis.
- Hematologic Effects: Rarely, cephalosporins can cause hematologic side effects, such as neutropenia, thrombocytopenia, and hemolytic anaemia. These effects are typically reversible upon discontinuation of the drug.
- Renal Toxicity: Some cephalosporins, particularly those eliminated by the kidneys, can cause renal toxicity, especially in patients with pre-existing kidney conditions. Monitoring renal function during treatment is essential to avoid potential complications.
Conclusion
Cephalosporins are one of the best lines of treatment in the fight against bacterial infections, offering a broad spectrum of activity and a relatively favourable safety profile. Their classification into different generations allows for targeted therapy based on the specific pathogen and infection type. However, like all antibiotics, cephalosporins should be used cautiously to avoid the development of antibiotic resistance. If you wish to stay updated with all things OPRA, visit Academically and check out our specialised preparation course to pass the exam in one go.