Epidemiology
Asthma is one of the most common non-communicable chronic diseases. It is more commonly seen in children than in adults.
The prevalence of asthma varies significantly across different regions of the world due to unique genetic, environmental, and occupational risk factors. However, this gap seems to be narrowing as asthma rates in high-income countries stabilise while they continue to climb in low- and middle-income countries.
Globally, an estimated 334 million people are currently living with asthma, and the disease is responsible for 250,000 deaths annually. The number of people affected by asthma is on the rise, with the total prevalence expected to increase by 100 million by 2025.
Causes
Many factors have been linked to an increased risk of developing asthma, though identifying a single direct cause is often challenging.
- Asthma is more likely if other family members have it, especially a close relative like a parent or sibling.
- People with other allergic conditions, such as eczema and rhinitis (hay fever), are more prone to asthma.
- Urbanisation is linked to higher asthma prevalence, likely due to various lifestyle factors.
- Early life events affecting lung development can increase asthma risk. These include low birth weight, prematurity, exposure to tobacco smoke and other air pollutants, and viral respiratory infections.
- Exposure to various environmental allergens and irritants, including indoor and outdoor air pollution, house dust mites, moulds, and occupational exposure to chemicals, fumes, or dust, elevates asthma risk.
- Overweight or obese children and adults are at a greater risk of developing asthma.
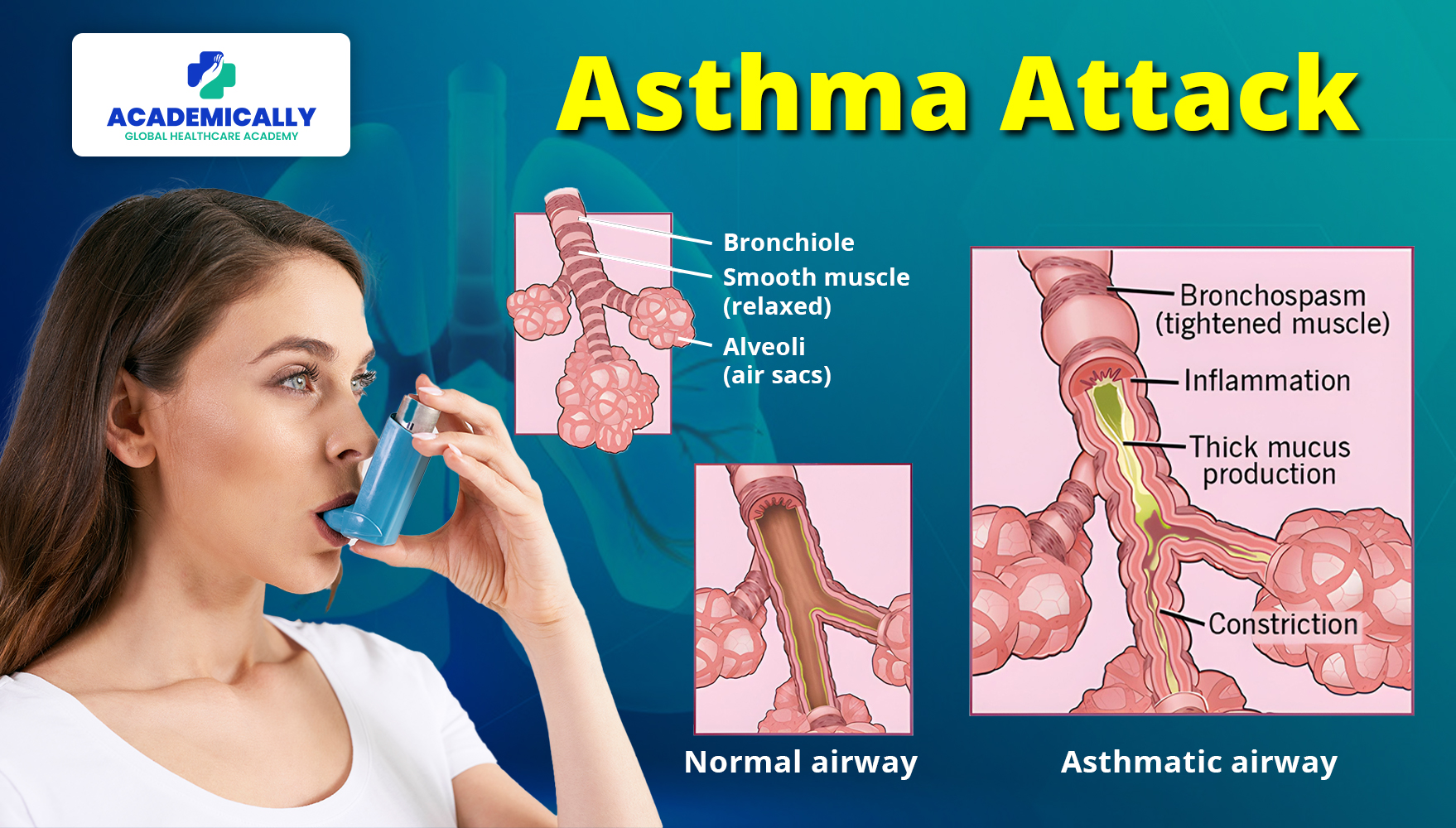
Symptoms
Asthma symptoms can vary widely among individuals and may worsen significantly during an asthma attack. These symptoms often intensify at night or during physical exertion.
Common symptoms of asthma include:
- Persistent nighttime coughing
- Wheezing during exhalation and sometimes inhalation
- Difficulty breathing or shortness of breath, which can occur even at rest
- A feeling of tightness in the chest, making deep breathing challenging
- Some people experience worse symptoms when they have a cold or during changes in the weather. Other triggers include dust, smoke, fumes, grass and tree pollen, animal fur and feathers, strong soaps, and perfume.
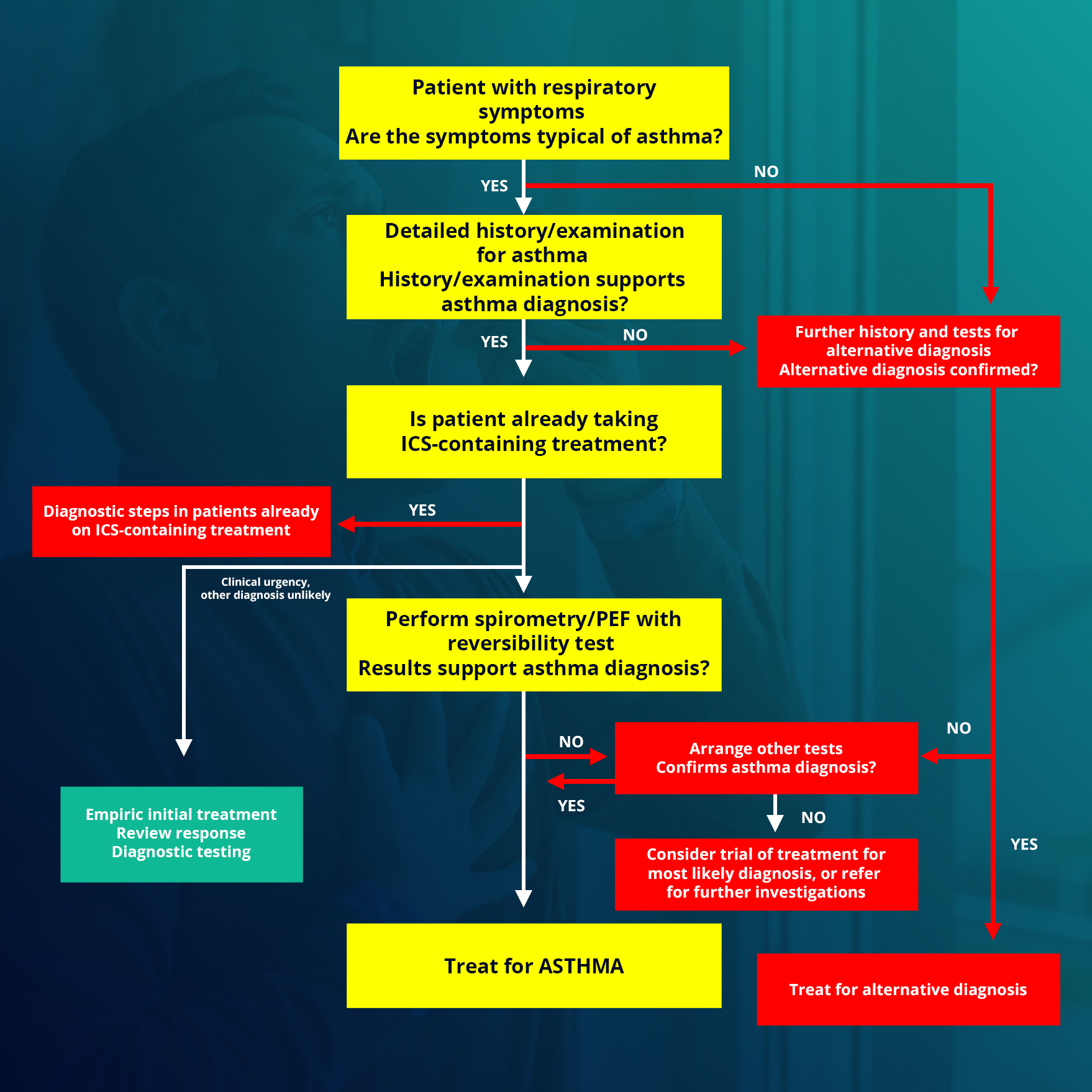
Diagnosis
An asthma diagnosis is confirmed through:
Medical History
A patient is more likely to exhibit asthmatic symptoms if there is a family history of asthma or allergies.
Physical Assessment
- Examination of the patient’s nose, throat, and upper airways for signs of asthma or allergies.
- Evaluation of respiratory rate and breathing patterns, including auscultation.
- Symptoms such as wheezing (high-pitched whistling sounds during exhalation), coughing, chest tightness, shortness of breath (SOB), runny nose, and swollen nasal passages are assessed.
Diagnostic Tests
The diagnostic tests to assess the patient’s breathing and monitor the effectiveness of asthma treatment are:
Lung Function Tests
- Spirometry
- Peak flow testing
Other Tests
- Allergy testing
- Bronchoprovocation
- Chest X-ray
- Electrocardiogram (ECG)
Treatment
The primary goal of asthma treatment is to control symptoms, prevent exacerbations and lung function loss, and reduce mortality.
1. Medications
The choice of medication depends on the disease's severity:
- For mild, occasional symptoms: Short-acting β2-agonists are effective.
- For long-term control: Inhaled steroids (oral steroids for severe cases) and long-acting β2-agonists are used.
- For acute exacerbations: Oxygen, short-acting β2-agonists, inhaled anticholinergics, and systemic steroids are administered.
2. Mechanical ventilation may be needed for severe exacerbations unresponsive to medical treatment.
3. Non-pharmacological measures, such as smoking cessation and avoiding occupational sensitisers, are crucial.
4. Asthma education on inhaler technique and self-monitoring is vital for effective asthma control.
Physiotherapy Management
1. Breathing Retraining Techniques
These techniques are particularly beneficial for mild to moderate asthma. The goal is to normalise breathing patterns by stabilising the respiratory rate and increasing expiratory airflow. Instructions include:
- Decreasing breaths taken (reducing respiratory rate)
- Taking smaller breaths (reducing tidal volume)
- Deep breathing (diaphragmatic breathing using abdominal muscles and lower thoracic chest movement)
- Breathing through the nose (nasal breathing)
- Relaxation (relaxed, controlled breathing)
- Decreasing air leaving (decreased expiratory flow through pursed lip breathing)
These techniques help control breathing and reduce airflow turbulence, hyperinflation, variable breathing patterns, and anxiety.
2. Buteyko Breathing Technique
This technique focuses on reducing hyperinflation and was developed based on the theory that hyperventilation leads to asthmatic bronchospasm. The method involves:
- Breathing normally through the nose for 2-3 minutes.
- Breathing out normally, then closing the nose with fingers and holding the breath.
- Recording the number of seconds until the first need to breathe (Control Pause).
- Returning to nasal breathing and waiting 3 minutes before repeating and holding the breath as long as possible (Maximum Pause).
The Buteyko technique aims to increase the control pause to 60 seconds and the maximum pause to 2 minutes. It is practised twice daily with a qualified practitioner to ensure safety. It aims to reduce respiratory rate and minute volume, increase carbon dioxide levels, and decrease bronchospasm.
3. Physical Training
4. Respiratory Muscle Training
Hyperinflation in asthma increases lung volume and alters inspiratory muscle mechanics, necessitating the use of accessory muscles. Breathing exercises with external devices make breathing more difficult, thereby strengthening inspiratory muscles. This results in easier diaphragmatic breathing and reduced hyperinflation. The breathing device sets up a load to breathe against, forcing the respiratory muscles to work harder and increase their strength.
5. Removal of Secretions
Techniques like percussions, shaking, vibrations, postural drainage, and effective coughing are used to mobilise and remove secretions. A randomised crossover study showed that physiotherapy maneuvers could safely induce sputum in well-controlled asthmatic children and adolescents, mobilising secretions without causing bronchospasms.
Final Words
Asthma is a common chronic condition that causes airway narrowing, obstruction, and mucus production, leading to breathing difficulties, coughing, wheezing, and shortness of breath.
The causes, epidemiology, symptoms, diagnosis, diagnostic test, and treatment are all important for healthcare professionals preparing for the exam.
Physiotherapy management is an important part of APC Exam Preparation. Make sure you don’t miss out this. For more study resource for the Australian Physiotherapy Council (APC) Exam, fill out this form.
For more such informational and educational materials, check our Instagram.